Understanding Medications Potentially Linked to Lymphoma
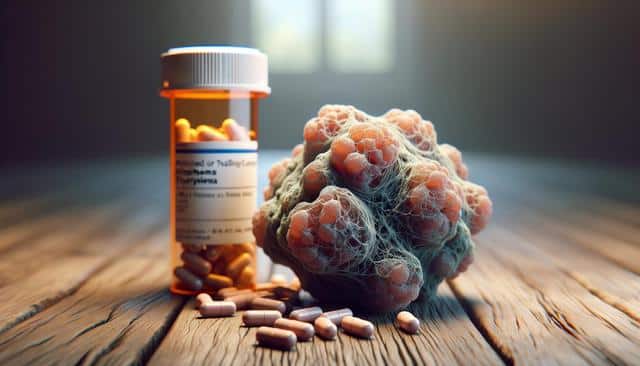
What is Lymphoma and Why Medication Links Matter
Lymphoma is a type of cancer that originates in the lymphatic system, which is part of the body’s immune defense. It primarily affects lymphocytes, a type of white blood cell. There are two main categories of lymphoma: Hodgkin lymphoma and non-Hodgkin lymphoma. While the exact causes of lymphoma can be complex and multifactorial, including genetic predisposition and environmental exposures, research has increasingly focused on the role some medications may play in elevating risk levels.
Certain prescription drugs, particularly those used to treat autoimmune conditions or suppress the immune system, have drawn attention due to observed associations with lymphoma in clinical studies. Understanding these links is crucial for patients and healthcare providers when evaluating treatment options, especially for long-term use. Although the presence of a link does not confirm causation, awareness can lead to more informed medical decisions and better risk-benefit analysis.
Immunosuppressive Medications and Their Role
Immunosuppressive medications are often used to manage conditions like rheumatoid arthritis, lupus, inflammatory bowel disease, and to prevent organ transplant rejection. These drugs work by dampening the immune system’s activity to prevent it from attacking the body’s own tissues. However, this suppression can reduce the body’s ability to detect and destroy abnormal cells, which may increase the risk of developing cancers such as lymphoma.
Some types of immunosuppressive drugs that have been examined in this context include:
- Calcineurin inhibitors
- TNF-alpha inhibitors
- Antimetabolites
- Monoclonal antibodies
Studies have suggested that long-term use or high dosages of these drugs may correlate with a higher incidence of lymphoma, particularly non-Hodgkin lymphoma. However, the risk level can vary depending on the specific medication, dosage, and patient health factors. Patients are encouraged to have regular screenings and open discussions with their healthcare providers about any associated risks.
Biologic Therapies and Targeted Treatments
Biologic therapies, a class of drugs that are genetically engineered to target specific components of the immune system, have revolutionized treatment for many chronic diseases. These medications, while often effective, can also inadvertently affect the body’s natural defenses against malignancies. Several biologic agents have been studied for potential links to lymphoproliferative disorders, including lymphoma.
Examples of biologic therapies under scrutiny include:
- Interleukin inhibitors
- B-cell depleting agents
- Checkpoint inhibitors
The mechanisms by which these drugs might contribute to lymphoma risk involve altering immune surveillance and potentially encouraging abnormal lymphocyte proliferation. While these medications can be highly beneficial for managing disease symptoms and progression, they must be prescribed with an understanding of the patient’s cancer risk profile, especially for those with a personal or family history of lymphoma.
Medications for Chronic Inflammatory Conditions
Individuals with chronic inflammatory conditions often require ongoing treatment, which may include non-biologic disease-modifying antirheumatic drugs (DMARDs) and corticosteroids. While these medications are effective at controlling inflammation, there is ongoing research into how their long-term use may impact cancer risk, including lymphoma.
Some potential concerns include:
- Prolonged immune system suppression that could reduce the body’s ability to monitor abnormal cell growth
- Inflammation itself acting as a co-factor in cancer development
- Combination therapy potentially amplifying risks
It is not always clear whether the elevated lymphoma risk is due solely to the medication or a combination of medication and the underlying condition. Nonetheless, strategies such as using the lowest effective doses, regular monitoring, and lifestyle adjustments can help mitigate potential risks over time.
Regulatory Warnings and Ongoing Research
Regulatory agencies worldwide continue to monitor the safety profiles of medications, including their potential cancer risks. In some cases, warnings have been issued about certain drugs that may increase the likelihood of developing lymphoma, particularly when used over extended periods. These warnings are based on clinical trials, post-marketing surveillance, and population studies.
However, it’s important to emphasize that regulatory advisories are typically precautionary measures. They are designed to inform healthcare providers and patients, not to discourage use of medications that may be necessary for managing serious health conditions. Ongoing research in this area includes:
- Longitudinal studies tracking patients over many years
- Clinical trials comparing various treatment regimens
- Genetic studies identifying individuals who may be more susceptible to drug-induced cancers
As research evolves, new insights will help refine treatment approaches and improve safety guidelines. Patients should stay informed and consult their physicians regularly to ensure that their treatment plans are both effective and aligned with the most current medical evidence.
Conclusion: Informed Decisions and Ongoing Dialogue
While some medications have been linked to a heightened risk of lymphoma, the decision to use them should be based on a comprehensive evaluation of the benefits versus the risks. For individuals managing chronic illnesses, these drugs often provide significant relief and improved quality of life. The key lies in maintaining an ongoing dialogue with healthcare providers, staying up-to-date with medical research, and tailoring treatment plans to each individual’s health profile and risk factors.
By understanding potential risks and working collaboratively with medical professionals, patients can make informed choices that support long-term health and well-being.