What Is Mycosis Fungoides?
Mycosis fungoides is a rare form of non-Hodgkin lymphoma that primarily affects the skin. It originates from a type of white blood cell called a T-cell, which normally helps fight infections. In this condition, the T-cells become cancerous and move to the skin, causing a range of visible symptoms. Unlike other skin conditions, mycosis fungoides develops slowly, often over many years, and can easily be mistaken for eczema or psoriasis in its early stages. Understanding its characteristics can help differentiate it from more common skin issues.
This disease typically begins with subtle signs that may not immediately raise concern. In the early stages, it often presents as flat, scaly patches that may be slightly itchy. These patches might appear reddish or pink and can be mistaken for chronic dermatitis. As the disease progresses, the appearance of the skin changes, becoming more pronounced and eventually forming tumors or thickened plaques. The slow progression underscores the importance of monitoring persistent skin changes and seeking medical evaluation when necessary.
Early Stage Appearance
In the initial phase, also known as the patch stage, mycosis fungoides may manifest as dry, slightly wrinkled areas of skin. These patches can vary in color from pink to reddish-brown and are often found on the lower abdomen, thighs, buttocks, and breasts. The affected areas might:
- Be slightly itchy or completely asymptomatic
- Appear flat and blend with surrounding skin
- Vary in size, from small spots to larger patches
Because of the mild nature of the symptoms, many individuals might not seek medical attention right away. The patches may come and go, further contributing to the confusion with benign skin conditions. However, if these patches persist or spread, it’s advisable to consult a dermatologist for proper evaluation and possible biopsy.
Progression to Plaques
As mycosis fungoides advances, the patches may evolve into plaques. Plaques are thicker than patches and often have a more pronounced color and texture. These lesions may be:
- Raised and scaly
- More intensely colored, often red or purple
- Accompanied by increased itching or discomfort
At this stage, the skin changes become more noticeable and may cover larger areas of the body. The plaques can sometimes crack or bleed, especially if scratched. Unlike patches, plaques tend to be more persistent and are less likely to fade without treatment. This stage is more likely to prompt individuals to seek medical help, which is critical for diagnosis and management.
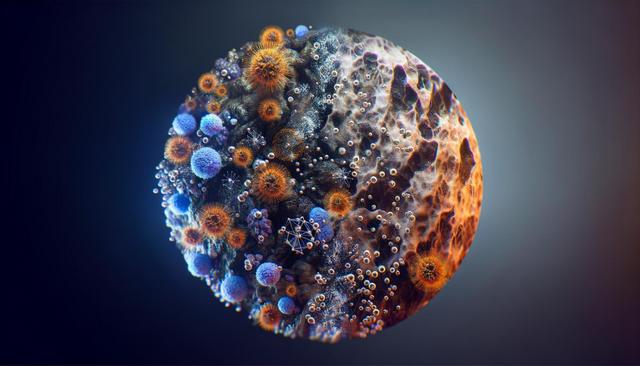
Tumor Stage and Advanced Symptoms
In more advanced cases, mycosis fungoides can progress to the tumor stage. Tumors are typically larger, nodular growths that may form on previously affected areas or new parts of the skin. These tumors can:
- Range in color from red to dark brown
- Be soft or firm to the touch
- Occasionally ulcerate or become infected
At this point, the disease may spread to lymph nodes, blood, or internal organs. The skin may become more fragile and prone to secondary infections. It’s also possible for multiple tumors to appear simultaneously, significantly affecting quality of life. Treatment becomes more complex in this stage and often involves a multidisciplinary approach including dermatologists, oncologists, and other specialists.
Importance of Medical Evaluation
Because mycosis fungoides mimics many benign skin conditions, a proper diagnosis often requires a skin biopsy and histological analysis. If you or someone you know has persistent or unusual skin lesions that do not respond to conventional treatment, it is essential to consult a healthcare provider. Common steps in the diagnostic process include:
- Physical examination and medical history review
- Skin biopsy to examine abnormal T-cells
- Blood tests and imaging for staging in advanced cases
Early diagnosis can significantly improve the management of mycosis fungoides. While there is currently no known cure, many patients manage the condition effectively with treatments such as topical corticosteroids, phototherapy, or systemic therapies depending on the stage. Awareness of the visual signs and persistent nature of this condition can lead to earlier detection and better outcomes.
Conclusion: Staying Informed About Skin Health
Recognizing what mycosis fungoides looks like can make a meaningful difference in how quickly it is diagnosed and treated. While it often resembles other chronic skin conditions in its early stages, paying attention to persistent or evolving skin changes is key. Individuals experiencing unexplained skin lesions or patches that do not resolve with typical treatments should consider seeking a professional evaluation. Early attention to skin abnormalities promotes better health outcomes and helps ensure timely interventions when necessary.



Leave a Reply